Transforming Healthcare Reimbursement with AI
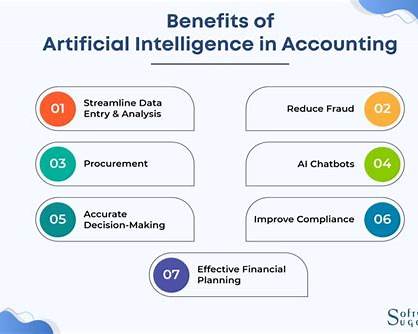
The introduction of an AI-driven fraud detection system marks a turning point in the healthcare industry's fight against fraudulent reimbursement claims. As the sector continues to embrace digital transformation, the adoption of artificial intelligence (AI) and machine learning (ML) has become crucial in ensuring the accuracy and efficiency of healthcare processes. This new system is designed to detect and prevent fraudulent activities in real-time, providing a robust solution to one of the industry's most persistent challenges.
Healthcare fraud not only leads to significant financial losses but also damages the reputation of organizations and invites regulatory scrutiny. The newly launched AI-powered system addresses these issues head-on by leveraging advanced technologies to monitor and analyze claims, identify suspicious activities, and prevent fraudulent transactions before they can occur. This approach represents a major shift from traditional methods, which often relied on manual review and were prone to human error.
Cutting-Edge Technology at the Core
At the heart of this innovative fraud detection system are advanced AI and ML algorithms that continuously learn and adapt to detect new types of fraud. This ensures that the system remains effective in identifying and mitigating emerging threats. The system's real-time analysis capabilities allow it to instantly evaluate claims upon submission, triggering automated alerts when suspicious activities are detected.
One of the key features of this AI-powered platform is its ability to recognize patterns commonly associated with fraudulent claims. For example, the system can detect inflated claim amounts, duplicate submissions, and pricing discrepancies, which are often indicative of fraud. Additionally, the system monitors user behavior to identify anomalies that may suggest fraudulent activity, providing an added layer of security.
The integration of AI in healthcare reimbursement is not only about detecting fraud but also about enhancing the overall efficiency of the claims process. By eliminating the need for constant manual review, the system saves time and reduces administrative burdens for healthcare providers and insurers. This, in turn, allows them to focus on delivering high-quality care to patients, rather than being bogged down by paperwork and fraud investigations.
Real-World Impact: Cost Savings and Enhanced Trust
The implementation of this AI-powered fraud detection system has already shown remarkable results in reducing costs and improving the integrity of the reimbursement process. By combining an extensive cashless network with advanced fraud detection capabilities, the system has the potential to cut costs by up to 20%. This substantial saving is achieved through a dual approach: a 10% reduction via the cashless network and an additional 10% through AI-driven fraud detection.
In practical terms, this translates to significant financial benefits for corporations and insurers. For instance, within a single policy year, the system helped reduce costs by ₹6.3 crore, demonstrating its effectiveness in a real-world setting. These savings not only enhance the financial stability of healthcare organizations but also contribute to a fairer and more transparent system for all stakeholders involved.
Moreover, the system's ability to detect and prevent fraud before it occurs helps build trust among patients, healthcare providers, and insurers. By ensuring that only legitimate claims are processed and paid, the system fosters a more secure and reliable reimbursement process, ultimately benefiting everyone involved in the healthcare ecosystem.
The Future of Healthcare Reimbursement
The launch of this AI-powered fraud detection system signals a new era in healthcare reimbursement, one where technology plays a central role in ensuring fairness, efficiency, and security. As AI and machine learning continue to evolve, we can expect even more sophisticated solutions to emerge, further enhancing the way healthcare providers, insurers, and patients interact with the system.
Looking ahead, the integration of AI into healthcare processes will likely expand beyond fraud detection, encompassing areas such as patient care, diagnostics, and personalized treatment plans. As these technologies become more widespread, they will play a crucial role in transforming the healthcare landscape, making it more efficient, cost-effective, and patient-centric.
In conclusion, the introduction of this AI-powered fraud detection system represents a major advancement in the healthcare industry. By harnessing the power of artificial intelligence and machine learning, the system not only combats fraud but also streamlines the reimbursement process, ensuring that healthcare providers and patients can focus on what truly matters—delivering and receiving high-quality care. This development sets the stage for a future where technology drives positive change across the entire healthcare ecosystem.